Pre-AEP Guidance
Pre-AEP is the timeframe between October 1 and October 14. During Pre-AEP, agents are allowed to set appointments, present plan benefits for the upcoming plan year, assist beneficiaries in completing a paper application, and/or send wet-sig applications when requested by the beneficiary. Allowable activities include: meeting with beneficiaries, assessing their needs, reviewing plan changes and options, giving a full sales presentation, and recommending coverage that will best meet the beneficiaries’ needs for the next plan year.
Agents must not encourage completion, solicit, accept, take possession of, or “just hold on to” any applications (paper or electronic) for the 2024 plan year prior to the start of AEP on October 15, 2023.
During Pre-AEP, agents can include their name and SAN on applications. DO NOT put a date next to agent name…. as this indicates when the agent took possession of the application even if the agent didn’t.
Per CMS guidelines, Humana/CarePlus must investigate any applications that come in with an agent name or SAN prior to the start of AEP for potential solicitation. Additionally, Humana will deny any applications where there is a Pre-AEP agent date on the application.
What Does This Mean to Agents
- You may place your name and SAN on applications
- Very Important! Do NOT date the application
- Agents may NOT EHub to “hold onto” applications until October 15
- Be thorough in reminding clients NOT to mail the application until October 15
- Humana field agents are encouraged to use the sticker provided in the Humana sales kit and place it on the business reply envelope to remind clients when to mail the application. We encourage you to have them initial next to the statement indicating that they understand.
- CarePlus agents can have the beneficiary initial next to the statement printed on the business reply envelope.
- Investigations will occur, and depending on the outcome, could result in corrective action up to and including termination of contract or employment.
Frequently Asked Question
Q: Can an agent who presents to a beneficiary during the Pre-AEP period over the phone, complete a paper app for the beneficiary during the call? The agent would then mail the application for signature and instruct the beneficiary to mail the application in after 10/15.
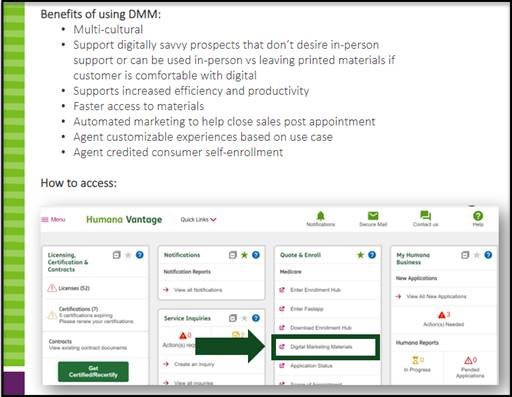
A: No. Agents are allowed to market plans during the Pre-AEP period, but they are not allowed to solicit applications, which in this case would include completing an application on behalf of the beneficiary. What the agent may do is present the plan over the phone and mail a sales kit that contains the paper application with the agent’s name and SAN number pre-filled in, with the rest of the application remaining blank for the beneficiary to complete. Alternatively, the agent may send the beneficiary a link through DMM where they can quote up to three (3) different plans, and the beneficiary has the option to complete the application once AEP begins. More should be available on MarketPoint University on Vantage. We also have this DMM video (https://vimeo.com/742821799/766a323e33) that helps break down the tool as well.
SEP for Dual-Eligible and LIS Individuals
CMS Chapter 2 guidance states those who are Dual-Eligible or receiving Low-Income and have not had a change in level may enroll, disenroll or switch to another Part D plan (either a PDP or MAPD) once per calendar quarter during the first nine months of the year. This means they may only make one plan change during each of the following time periods:
- January – March
- April – June
- July – September
What Does This Mean to Agents
During the 4th quarter (October – December), Dual Eligibles and those receiving LIS/Extra Help who have not had a change in level and wish to make a plan change must use the Annual Enrollment Period (AEP) election code. The MDE election code MAY NOT be used during the 4th Quarter, including the timeframe outside of AEP from 12/8 – 12/31. You are also NOT permitted to select SEP-OTH and write in “LIS”, “Medicaid”, “Extra Help” or similar verbiage.
SEP for Those with a Gain, Loss, or Change in Status
We want to remind you that there are separate SEPs for those individuals who gain, lose or have a change in their Medicaid or LIS/Extra Help status. These SEPs allow those individuals one opportunity to make an election within three months of the status change and it does not count towards the once per calendar quarter limitation.
Election Codes to Use on the Application
Medicaid Enrollees = Use MCD
Extra Help Enrollees = Use NLS

